Getting It Right the First Time: Empowering clinicians with insights & training for inclusive paediatric care
The NHS Getting It Right the First Time (GIRFT) programme emphasises the need to reduce variations in service delivery to improve patient care and outcomes, as well as deliver efficiencies by reducing costs and unnecessary/repeat procedures.
The Challenge: Gaps in Pre-Appointment Insight
In paediatrics, “getting it right” often depends on understanding each child as an individual before the appointment even begins. The current gaps in pre-appointment insights leave clinicians facing a difficult balancing act: delivering personalised, compassionate care within the constraints of short, fast-paced appointments. Building rapport, understanding sensory or communication needs, and anticipating emotional triggers often have to happen in minutes.
Yet these insights are what make care effective. Without them, even routine appointments can feel overwhelming for children and families - especially for neurodivergent children, for whom unfamiliar environments and unpredictable experiences can cause distress (You can read more about our insights from 158 families on accessing healthcare as a neurodiverse child). The impact of one bad experience goes beyond a single appointment: when children feel anxious or misunderstood, their confidence in healthcare can reduce, shaping how they engage with services in the future.
Our mixed-methods research with 40 clinicians - including interviews, observations, and a survey -highlighted the gaps, challenges, and opportunities to use digital health innovation to align everyday clinical practice with GIRFT’s aims of efficiency, quality, and consistency.
The Current Landscape: Fragmented and Incomplete Information
Our research indicates clinicians mainly receive patient information through electronic health records (EHRs) or written forms. While EHRs are preferred by 68 % of respondents, their content often lacks nuance.
Clinicians said they ideally want:
- A short parent-completed questionnaire that provides direct insight into a child’s current needs.
- A summary from previous clinicians to build continuity across care settings.
- Integration with existing EHRs or, where not feasible, a quick-reference PDF report.
But across hospitals, systems are fragmented. Some clinicians rely on paper forms or informal notes that don’t reliably reach the right people.
Why Pre-Appointment Insight Matters
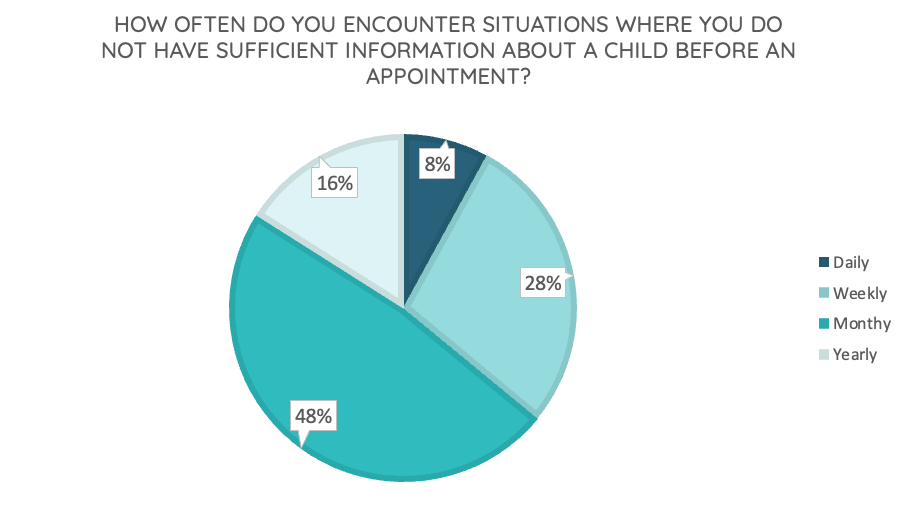
Every clinician we spoke to agreed that pre-appointment insight is essential; 80 % said it is very important. Yet 90 % reported working with insufficient information at least monthly, and a third said this happens weekly.
These gaps leave clinicians managing complex emotional and behavioural needs without the necessary context to make compassionate care possible. Many described child and adolescent anxiety, especially post-pandemic, as a growing issue. Few had formal training in supporting neurodivergent children and instead learned “on the job.” Junior clinicians often felt “unsure,” “anxious,” or even “scared” in these scenarios.
That’s why, alongside building better tools to gather and share insights, training is crucial. In a 2023 study, 100% of healthcare professionals sited the need for more training as a main concern when taking care of patients with autism.
To help close this gap, we’ve developed a free CPD course that gives clinicians practical strategies for supporting neurodivergent patients - complementing tools like A Little About Me and directly advancing GIRFT’s focus on reducing unwarranted variation in care quality.
Beyond the Numbers: How Insight Enables Compassionate Care
Clinicians consistently told us that pre-appointment information is essential. But what really stood out in our research was why this matters. It’s not about having more data; it’s about having the right context to make informed, compassionate decisions under pressure to deliver the best outcomes for every patient.
Without insight into emotional triggers or communication preferences, even experienced clinicians can be caught off guard. One anaesthetist described the risk of misjudging a child’s needs based on surface behaviour:
“If you go into a room and a child is quiet and seems compliant, you might not think they need a pre-med. But if that quiet child then goes on to have a meltdown, you are not prepared.”
With the right information in advance, clinicians can make small but powerful adjustments, such as changing the order of procedures, adapting lighting, or even wearing a hoody over their uniform where appropriate if that helps the child feel safe.
“If uniforms are triggering for a child, I need to know the day before so I can bring in a hoody to work.”
Rapport-building was another recurring theme. Clinicians can often use humour or shared interests to connect with children quickly, transforming a clinical interaction into a moment of trust. As one clinician put it:
“Even knowing what football team they like, I would do a quick Google before going into the room—just to know what league they are in.”
These details help strengthen the bond between clinicians and patients, supporting their emotional safety.
The crucial role of the caregiver
Finally, clinicians emphasised the importance of understanding caregiver needs. Caregiver anxiety can be a key determinant of child anxiety, yet their needs are often overlooked in paediatric settings. By anticipating and addressing both sides of the care relationship, clinicians build trust and avoid tension. It’s not just about treating the child, it’s about supporting the whole family.
Together, these insights show that pre-appointment information is a clinical enabler. It helps clinicians feel confident, helps families feel seen, and helps children feel safe.
What Clinicians Want to Know
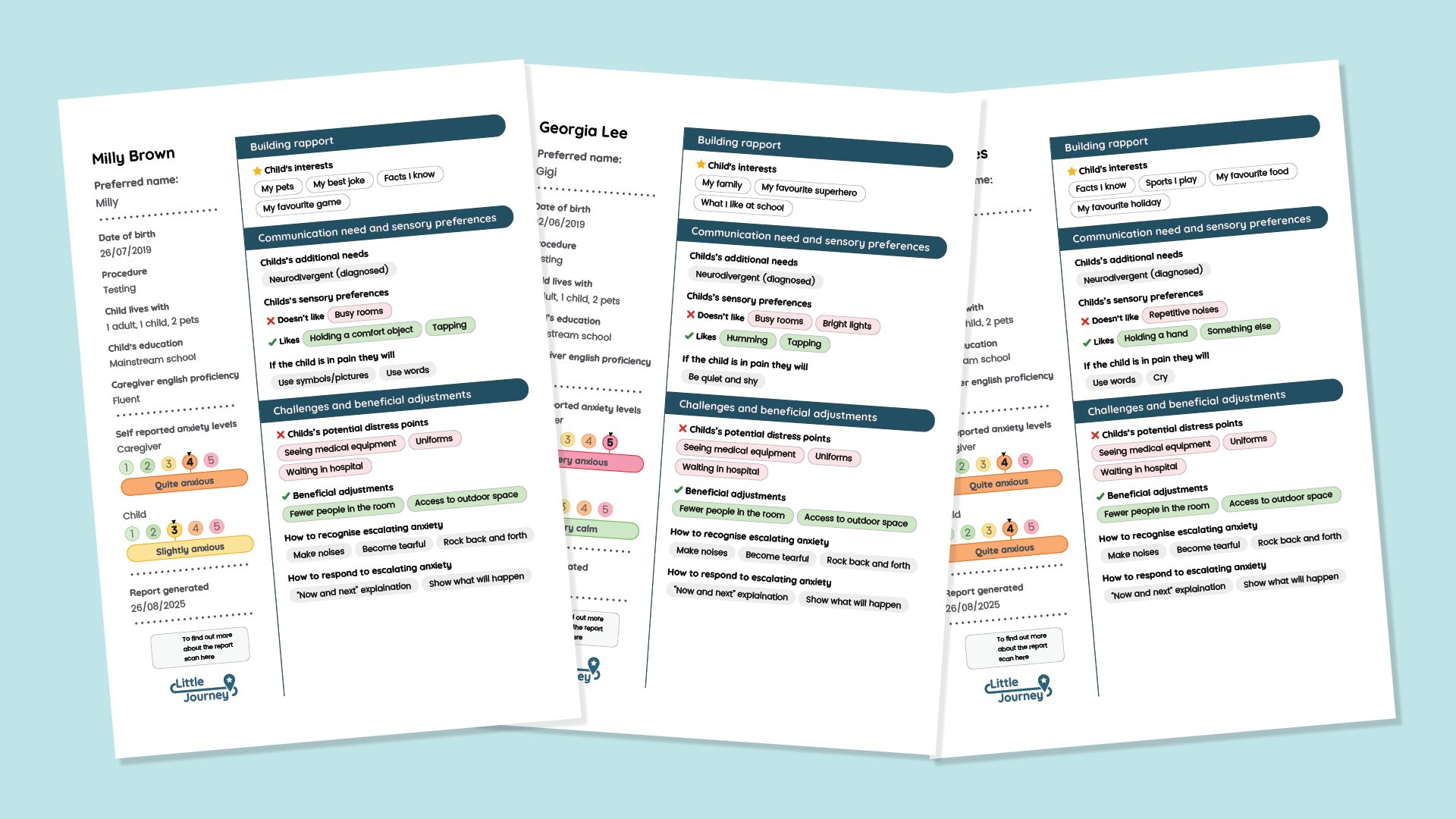
Before meeting a child, especially a neurodivergent child, clinicians prioritised understanding:
- Preferred name and interests (to build rapport)
- Communication and sensory needs (to tailor interactions)
- Triggers for distress (to anticipate challenges)
- Caregiver anxieties and previous hospital experiences (to anticipate challenges)
- Adjustment strategies (to reduce distress)

As one clinician put it, “Every neurodivergent child is different and not to make assumptions.” This quote highlights the challenge: without personalised insight, even the most experienced professionals risk missing what matters most.
However, they also flagged the need for balance. Too much information is overwhelming and hard to action; concise, descriptive insight was considered the most valuable.
Bridging the Gap: From Insight to Action
These findings reveal a clear opportunity to strengthen GIRFT objectives by giving clinicians consistent, actionable insight. What’s missing is a practical mechanism to collect and share that information across settings.
Designing A Little About Me care profiles with Clinicians in Mind
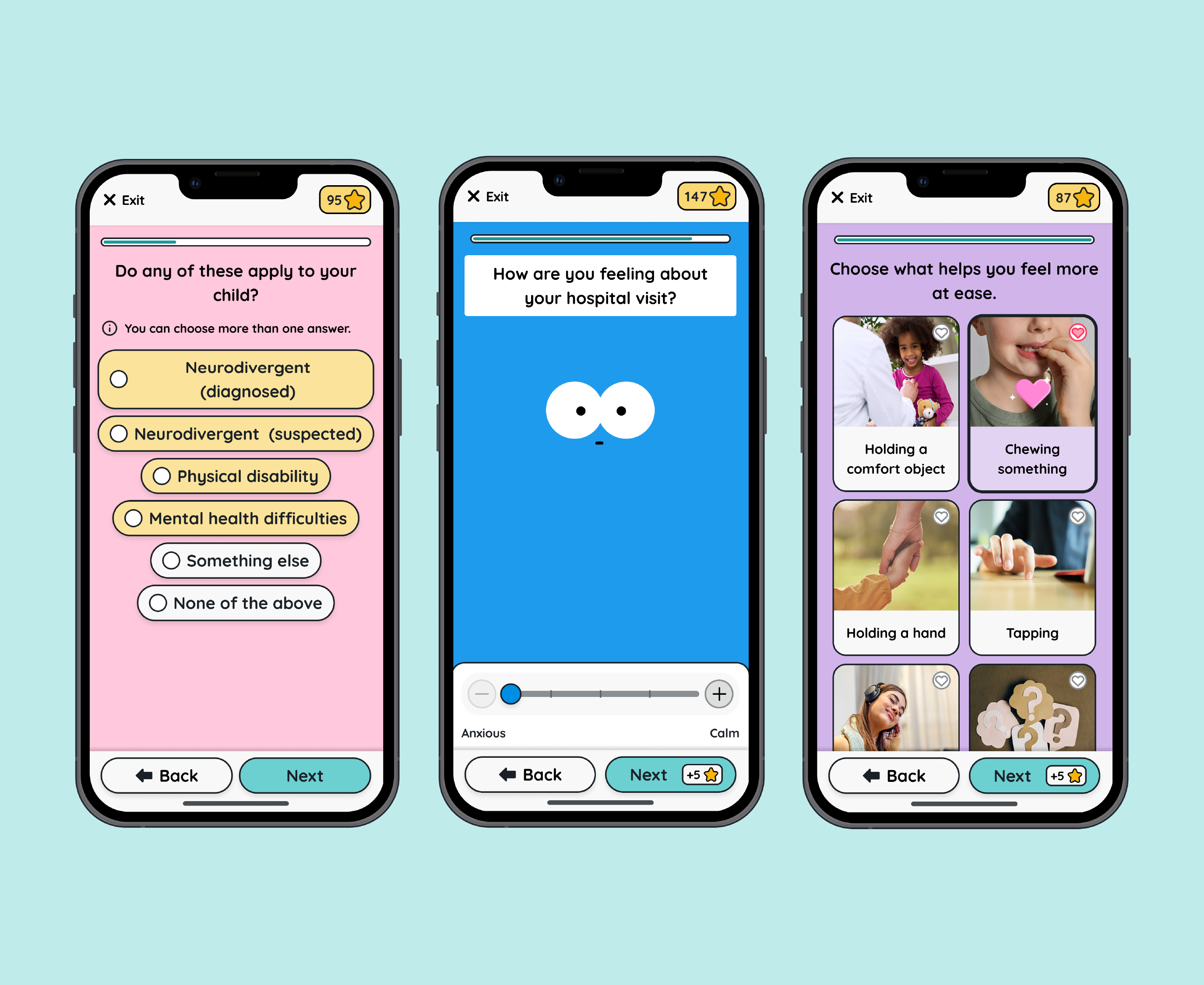
Drawing on the clinician insights, literature on procedural anxiety risk factors, collaboration with families and neurodivergent children, and the collective expertise of our team, we developed A Little About Me care profiles - a first-of-its-kind digital tool that gives children a voice in their own care - gathering pre-appointment insight and turning it into meaningful action.
At a Patient Level:
Interactive quizzes help children share preferences, potential triggers, and interests in accessible ways, empowering them to express their needs.
At a Provider Level:
A personalised care profile report is automatically generated - concise, practical, and actionable - so clinicians can quickly review to gain insights with no extra admin.
At an Organisational Level:
Care profiles enable staff to tailor their approach to each child. By embedding personalised insight into clinical workflows, A Little About Me helps standardise inclusive care across settings, ensuring that information about a child’s needs is consistently available, regardless of hospital culture, resources, or staffing.

Together, these levels advance GIRFT’s ambition to reduce variation and deliver efficient, high-quality, inclusive care.
Reimagining Neurodivergent Care Pathways
Tools like A Little About Me care profiles allow clinicians to “get it right the first time.” With actionable insight upfront, clinicians can make reasonable adjustments that ease anxiety, improve communication, and strengthen trust for individual patients. For neurodivergent children - who are twice as likely to experience procedural anxiety and five times more likely to require repeat visits - these adjustments can be transformative.
When used at scale, these care profile reports can drive better clinical decision-making, emotional safety, and smoother operational flow.
See It In Action: Free CPD Training and A Little About Me Demo
A Little About Me care profiles are now live for all our app for UK healthcare customers! If your hospital is not yet a Little Journey partner, speak to our team for a demo of the care profiles module.
To complement this innovation, we invite healthcare clinicians to join our free CPD-accredited online training, designed to help professionals deliver more inclusive and compassionate care for neurodivergent children and their families.
The training explores what neurodiversity means in healthcare, the common barriers children may face, and practical strategies for change through the evidence-informed P.A.U.S.E. Framework. This framework promotes preparation, accessible communication, sensory awareness and adjustments, personalisation, advocacy, and empathy in care.
The benefits are shared: better experiences and outcomes for children and families, and more confident, effective, and efficient care for staff.
Get notified when new CPD modules are released
Together, we can ensure every child feels safe, seen, and supported—and that clinicians have the tools and training to truly get it right the first time.